Not all clinical trials are designed the same way or have the same objectives. Here, we’ll dissect the various types of clinical trials, their respective importance to research and development of new treatment tools, and their divergent methods.
What Are Clinical Trials and Why Are They Important?
Before we get into the different types of clinical trials, let’s briefly establish their basic purpose so that you can better understand the subtleties of the distinctions in varieties.
Clinical trials are an essential part of the research and development process to bring innovative new therapeutics, treatments, and medicines to American patients who benefit from them. All fields of medicine rely on them, including child neurology.
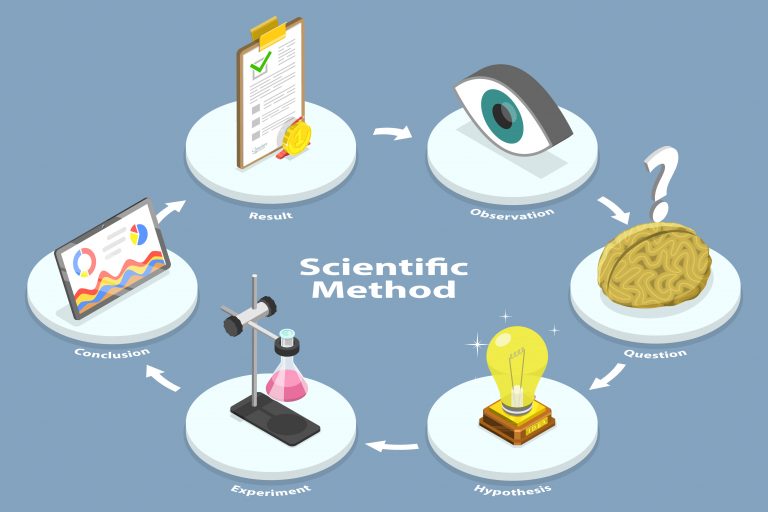
The research process for new treatments begins in a lab with a working hypothesis – but until new ideas are actually tested on humans, we have no real evidence that they will actually work as theorized.
Accordingly, depending on the type of trial, clinical testing helps researchers and drug companies:
- Establish baseline safety and efficacy of a new drug or treatment
- Identify and record potential side effects
- Find the optimal dosage
- Gain approval from the regulatory authorities (primarily the FDA) in the final stages
Interventional vs Observational Clinical Studies
Broadly speaking, clinical trials can be divided into two main types:
- Interventional clinical studies. “Interventional study designs, also called experimental study designs, are those where the researcher intervenes at some point throughout the study. The most common and strongest interventional study design is a randomized controlled trial, however, there are other interventional study designs, including pre-post study design, non-randomized controlled trials, and quasi-experiments.”
- Observational clinical studies. “Observational studies, also called epidemiological studies, are those where the investigator is not acting upon study participants, but instead observing natural relationships between factors and outcomes.”

Basically, interventional clinical studies aim to study a particular drug or treatment for a specific condition. Most often, these trials contain a “control” group that is not given the treatment or receives a fake treatment (a “placebo”) to compare the results later with the “intervention” group that received the genuine treatment under study.
To further enhance the accuracy of the trial, the researchers may also make the trial “blind,” meaning that patients and/or researchers (in the case of a “double-blind” model) don’t know who is receiving the real treatment and who is receiving a placebo.
The “gold standard” of clinical interventional studies is the randomized double-blind placebo control (RDBPC) model with high numbers of participants to filter out any confounding variables.
On the other hand, observational clinical studies do not involve any treatment, whether placebo or real. Instead, researchers simply observe (hence the name) participants and record the results. These studies can range in complexity and intensity from long-term studies using advanced medical testing on large populations to small-scale surveys.
Randomized vs Non-Randomized Interventional Clinical Studies
The decision of which treatments to give which participants in a clinical study has important implications in terms of interpreting the results and extrapolating the utility and safety of a new treatment for use in the general population.
Interventional studies fall into one of two categories related to allocation:
- Non-randomized. In non-randomized trials, researchers assign participants with interventions intentionally and are aware of who has received which treatments.
Randomized. In randomized trials, researchers determine which interventions to assign to which participants entirely randomly – by computer, coin toss, or other means. The key benefit of randomized trials is that they eliminate bias.

Both randomized and non-randomized studies have value:
“There is debate surrounding the optimal research design; however, both randomized and nonrandomized designs are important to build a broad, informative evidence base. The designs are therefore complementary, with unique advantages and limitations. The applicability of either approach hinges on the clinical question posed, the feasibility of studying it, and ethical considerations.”
It is not uncommon for researchers to use a combination of each type in a meta-analysis, which includes analyzing the results of multiple studies to determine a consensus outcome.
Different Models For Observational Studies: Cohort Studies vs Case Control Studies vs. Cross Sectional Studies
We can further divide observational clinical trials into three distinct categories: cohort, case control, and cross-section:
- Cohort studies include groups of people whose health outcomes are monitored over set time periods, which puts them in a category called longitudinal studies. For example, in the context of child neurology, researchers might look at anxiety levels in children and how they change over time without any intervention.
- Case control studies are the methodological opposite of cohort studies. Like cohort studies, they include groups of people. However, the researchers select participants based on whether they have a given health condition or not, and then look back to see which participants were exposed to suspected risk factors and which weren’t. The advantage of case control studies over cohort studies is that they are cheaper and easier to conduct; however, they might not be as accurate.
- Cross section studies. Cross section studies look at data from participants gathered at a particular point in time rather than over a period of time. Because of the time factor, cross section studies are actually often the most affordable option available, although their accuracy is usually less solid than studies conducted over time, particularly compared to cohort studies. Often, cross section studies are preliminary before researchers begin more costly cohort or case control studies.
Feasibility and Pilot Studies
Frequently, the inaugural stages of clinical research call for feasibility and/or pilot studies. These are designed as exploratory measures to assess the potential of a newly designed treatment to actually work in real-world settings.
If the feasibility or pilot study indicates a strong potential for success, then the new therapeutic will pass on to the next stages which include larger-scale studies.

Here is how feasibility and pilot studies work:
- Feasibility studies explore whether a main study will be workable. It includes how well the efficacy and safety of a new treatment can be measured and recorded, whether doctors and patients can participate without any barriers, and how the information collected can be processed most efficiently. What feasibility studies do not offer is an answer to whether the treatment actually works.
- Pilot studies are miniature versions of later possible larger-scale tests. They are valuable for working out the logistics of the study and how all the working components interplay with one another. Importantly, pilot studies do attempt to answer the central research question about the safety and efficacy of the treatment at hand.
Learn More About Clinical Trials From Florida’s Leading Clinical Research Group
Parents may understandably have a lot of questions about clinical trials, how they work, and why they’re so important for the field of medicine. Please feel free to contact us; we’re always happy to further connect with our patients and their caregivers in Northwest Florida.